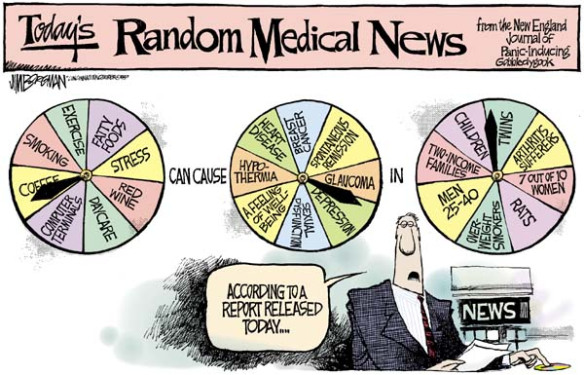
 Every prescription drug (or over-the-counter medication) in your bathroom cabinet is there because it’s been evaluated in research called a clinical trial. For a basic introduction to clinical trials, let’s turn to former editor-in-chief of the prestigious New England Journal of Medicine, Dr. Marcia Angell, who wrote the following in her frightening landmark piece called “Drug Companies & Doctors: A Story of Corruption” (New York Review of Books, 1/15/2009):
Every prescription drug (or over-the-counter medication) in your bathroom cabinet is there because it’s been evaluated in research called a clinical trial. For a basic introduction to clinical trials, let’s turn to former editor-in-chief of the prestigious New England Journal of Medicine, Dr. Marcia Angell, who wrote the following in her frightening landmark piece called “Drug Companies & Doctors: A Story of Corruption” (New York Review of Books, 1/15/2009):
“Before a new drug can enter the market, its manufacturer must sponsor clinical trials to show the Food and Drug Administration that the drug is safe and effective, usually as compared with a placebo or dummy pill.
“The results of all the trials (there may be many) are submitted to the FDA, and if one or two trials are positive – that is, they show effectiveness without serious risk – the drug is usually approved, even if all the other trials are negative.”

 There is strong evidence that medical researchers’ financial ties to their industry funders may directly influence their published positions in
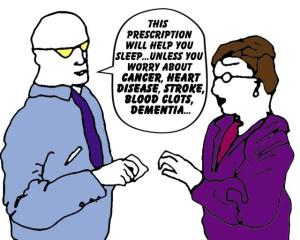
There is strong evidence that medical researchers’ financial ties to their industry funders may directly influence their published positions in I’m not a scientist. I’m merely a dull-witted heart attack survivor who started asking questions about the fistful of cardiac drugs I now have to take each day. But I did spend 20 years of my life living with a scientist, which meant countless scintillating breakfast table conversations on topics like zinc and copper sediment in the Fraser River estuary. (Does that count at all?)
I’m not a scientist. I’m merely a dull-witted heart attack survivor who started asking questions about the fistful of cardiac drugs I now have to take each day. But I did spend 20 years of my life living with a scientist, which meant countless scintillating breakfast table conversations on topics like zinc and copper sediment in the Fraser River estuary. (Does that count at all?) In case you believe that the medicine you’re taking has been adequately tested on real live patients before being legally approved, you might want to consider research published recently in The New England Journal of Medicine
In case you believe that the medicine you’re taking has been adequately tested on real live patients before being legally approved, you might want to consider research published recently in The New England Journal of Medicine